What is Fetal echocardiography or Fetal ECHO?
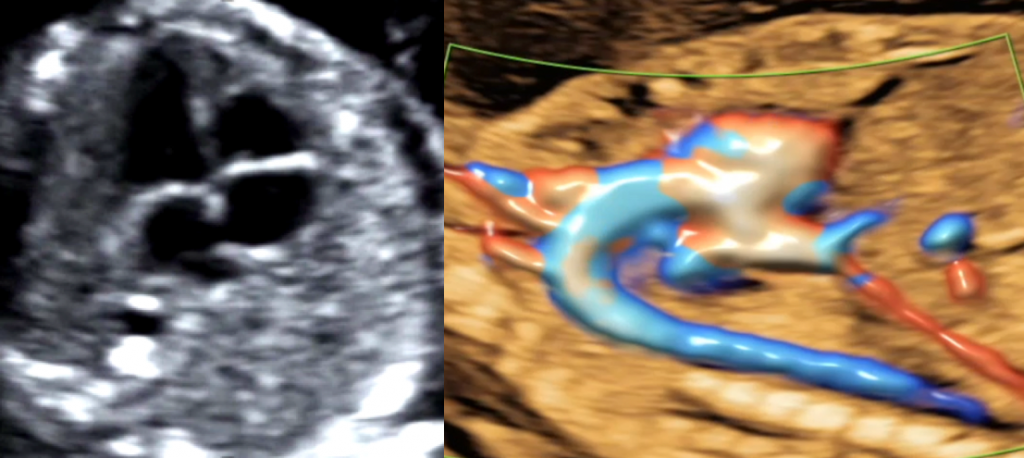
A Fetal echocardiography is an ultrasound scan performed during pregnancy to evaluate the fetal heart in detail.
Is a Fetal ECHO recommended in every pregnancy?
Every pregnant woman may not undergo a Fetal ECHO. It is recommended for woman falling under following categories
- Previous child was born with a heart defect
- Family history of genetic heart problems
- A chromosomal or genetic abnormality is discovered in the baby (such as, but not limited to, Trisomy 13, 18 or 21, also known as Down’s syndrome)
- Edema or abnormal fluid around the fetal organs (heart, skin, liver and lungs)
- If abnormalities of multiple organs, such as the kidney, bones or brain, are detected
- Fetal lung abnormalities, such as congenital diaphragmatic hernia, a lung malformation or a lung tumor
- Certain abnormalities in previous ultrasound scans or other blood tests
- Baby with too fast, too slow or irregular heartbeats on ultrasound scan
- Certain types of twin pregnancies (MCDA twin / Identical twins)
- Expecting mother has certain heart problems
- Maternal exposure to certain medicines during pregnancy that may cause congenital heart defects. These include certain medicines for seizures, depression, acne, anti-inflammatory (eg; Ibuprofane,indomethacin, etc.) and blood pressure medicines (ACE-inhibitors).
- Maternal alcohol or drug abuse during pregnancy
- Mother with health issues like diabetes, lupus (SLE) or phenylketonuria
- Maternal infections during pregnancylike German measles or Rubella, or cytomegalovirus (CMV), etc.
When is a Fetal ECHO performed?
The above are the indications for a detailed Fetal ECHO which is generally done between 18-24 weeks of pregnancy.
However, a basic Fetalehco is routinely performed as a part of a standard mid trimester anomaly scan done between 18-20 weeks. Now-a-days, a few major cardiac anomalies may be even detected as early as 12-14 weeks at the time of NT scan.However, the mother will likely be asked to return for more definitive scan later in gestation (18-24 weeks) to confirm the earlier findings.
Heart is an evolving organ which grows from a size smaller than that of a peanut (during NT scan) to a full-grown heart which is almost as big as the baby’s fist. It undergoes many changes throughout the course of pregnancy. Hence a detailed fetal cardiac evaluation is ideally recommended at every stage in pregnancy starting form as early as 12 weeks up till delivery. However, the evaluation of the fetal heart may become technically difficult and suboptimal during later stages of pregnancy owing to fetal position.
How is a Fetal ECHO performed and how should one prepare for this scan?
There are no special preparations required for this scan. It is generally a trans abdominal ultrasound which is performed just as any other routine abdominal pregnancy ultrasound scan. The only difference is that the focus of the examination is the fetal heart. Sometimes in early gestation, a trans vaginal scan may be required to evaluate the fetal heart in detail.
However, in this scan, the baby’s heart has to be seen and examined from very specific angles and hence this scan is highly dependent on the baby’s position. If the baby is not in an optimal position, one may have to wait till the baby moves, turns and decides to co-operate for the scan.
On an average, this scan takes somewhere between 30-120 minutes or sometimes even longer depending upon the baby’s position and the complexity of the heart problem.
Hence, it is highly recommended to fix a prior appointment for the scan and keep the entire day completely reserved for the baby without other commitments on that day. Have a good meal before the scan and carry some snacks along with you.
What should one expect after the scan?
A normal Fetal ECHO may be quite reassuring for the couple.
Whenever a heart problem is detected, the fetal medicine specialist will explain it thoroughly to the couple in simple language of their understanding. He will also discuss the possible implications that problem may have in the ongoing pregnancy, possible treatment options (before or after the birth of the baby) and possible outcomes.
The couple may be referred to a paediatric cardiologist or a paediatric cardiac surgeon to discuss whether or not the defect will impact the fetus prior to or after the birth, require immediate treatment after birth, require admission to the neonatal or cardiac intensive care unit (ICU) and/or require heart surgery after birth with possible post-natal (after birth) care, course and outcomes.
A fetal medicine specialist, paediatric specialist and the treating obstetrician will then take a decision regarding antenatal follow up and management in such cases which importantly includes time and place of the delivery. If a problem is detected, it is highly recommendedbe delivered in a tertiary hospital with expert neonatal and paediatric cardiac facilities available under the same roof. As these babies may require expert attention immediately after birth which can be lifesaving in most cases.
It’s important to note that even in the case of a normal fetal echocardiogram, the test has inherent limitations, as the blood circulation in the fetus is different than it is after birth. Some limitations include the inability to rule out small holes (such as atrial or ventricular septal defects), a pulmonary venous abnormality (also known as partial anomalous pulmonary venous return), minor valve abnormalities (including bicuspid aortic valve), and coarctation of the aorta. Despite these limitations, a normal fetal echocardiogram is largely reassuring of a very low likelihood of structural heart disease.